Find out about your options for head and neck cancer treatments, and complementary treatments that can be used alongside medical care.
Download the complete head and neck cancer booklet
Our new booklet 'Understanding head and neck cancer' is available now.
Download section five of our head and neck cancer booklet: Head and neck cancer treatments
- Talk to your treatment team about the things you can do before treatment starts to help with your recovery.
- Before any treatment begins, it is likely that you will need to see a dentist. The dentist will talk to you about how to care for your mouth before, during, and after treatment.
- Depending on the type and stage of cancer, treatment may include:
- surgery
- radiation treatment
- chemotherapy
- targeted treatment
- palliative care
- any combination of these.
- Many people use complementary, traditional Māori, or Pacific therapies alongside their hospital cancer treatment. While many of these therapies are safe to use while you are having hospital treatment, it is always best to discuss what therapies and treatments you are using with both your hospital treatment team and your therapist just to be sure.
- Kōrero ki tō kapa maimoatanga e pā ana ki ngā mea e āhei ana koe ki te mahi i mua i te tīmatatanga o te maimoatanga hei āwhina i tō whakaoranga.
- I mua i te tīmatatanga o ngā maimoatanga, kāore e kore me haere koe ki te kite i tētahi tākuta niho. Māna koe hei kōrero me pēhea te tiaki i tō waha i mua i te maimoatanga, i te wā o te maimoatanga, whai muri hoki i te maimoatanga.
- E ai ki tōna momo me te wāhanga kua eke te matepukupuku, tērā pea ka whāia ko ētahi o ēnei maimoatanga:
- Hāparapara
- Maimoatanga iraruke
- Hahau
- Maimoatanga whakahāngai
- Atawhai taurima
- He kōwhiringa o ēnei
- He maha ngā tāngata whakamahi ai i te haumanu tautoko, te haumanu Māori taketake, ngā haumanu Moana-nui-a-Kiwa rānei, i te taha o ngā maimoa matepukupuku o tō rātou hōhipera. Ahakoa he haumaru te nuinga o ēnei haumanu ki te whakamahi i te wā e whai maimoa ā-hōhipera koe, he pai ake ki te matapaki ko ēhea ngā haumanu, ngā maimoatanga e whakamahi ana koe i te taha o tō kapa maimoa hōhipera me tō kaiwhakatika, kia mōhio tūturu ai koe.

Before treatment starts
Before you are diagnosed with head and neck cancer, you may have already had problems with speech, swallowing, or the health of your teeth and gums.
Your recovery after treatment will depend on many factors. However, there are some things you can do before treatment starts to help in your recovery.
See a dentist
Before any treatment begins, it is likely that you will need to see a dentist. The dentist will talk to you about how to care for your mouth before, during and after treatment.
If you have tooth decay (holes in your teeth) or gum disease, this will need to be sorted before treatment (especially radiation treatment) can begin to reduce the risk of getting an infection.
Improve your diet and nutrition
If you are underweight or losing weight, try to eat good sources of protein and include high-energy (high-calorie) foods in your diet. Good sources of protein and energy include:
- meat, fish, and poultry
- milk and dairy products
- legumes e.g. baked beans, kidney beans, chickpeas, lentils and nuts.
If you have tried increasing your energy intake but still struggle to eat enough, you may benefit from a nutritional supplement drink. Talk with a dietitian or your treatment team to get the right supplement for your needs.
If you are unable to eat and drink, your treatment team may talk to you about having a PEG feeding tube placed into your stomach to help meet your nutritional needs.
Read more about eating well with cancer
Avoid or reduce alcohol
If you drink alcohol, stopping drinking or reducing the amount of alcohol you drink can help make your treatment more effective, and reduce the risk of side effects. If you would like support to reduce the amount of alcohol you drink, your treatment team, GP or whānau doctor can arrange this for you.
Increase your physical activity
Light exercise, such as walking, or keeping up your normal exercise routine will help build strength for your recovery. Do not start a new exercise programme without talking it through with your GP or whānau doctor first.
Read more about keeping active with cancer
Stop smoking
Current smokers should stop smoking as soon as possible. This will reduce the risk of complications immediately after surgery, help with your recovery after cancer treatment, and improve your heart and lung health. Stopping smoking will also reduce the risk of developing another cancer in the future.
Treatment options
Your cancer treatment team will advise you on the possible treatments for head and neck cancer. Depending on the stage of the cancer, your state of health, and your choices, treatment may include surgery, radiation treatment, chemotherapy, palliative care, or combinations of these.
| Mouth (oral) cancer |
Lips Tongue (oral) Gums Cheek Roof of mouth Floor of mouth |
|
| Nasal or paranasal sinus cancer |
Nose Paranasal sinuses |
|
| Salivary gland cancer |
Parotid Sublingual submandibular |
|
| Pharyngeal (throat) cancer |
Nasopharynx Oropharynx Hypopharynx |
|
| Laryngeal cancer |
Larynx |
|
| Skin | Pinna (outer ear) Scalp Face Neck |
|
| Thyroid | Thyroid |
|
Surgery
Many people with head and neck cancer have surgery. Your treatment team will discuss the best surgical options for you.
Surgery may be done for different reasons. You may have surgery to:
- completely remove the cancer
- remove lymph nodes if the cancer has spread to them, or if there is a chance
the cancer might spread to them - reduce pain or ease symptoms (palliative surgery)
- improve your appearance and ability to swallow and/or speak after treatment (reconstructive surgery).
The type of surgery you have will depend on the size of the cancer and where it is in your mouth.
Types of surgery include:
- glossectomy—removes all or part of the tongue
- mandibulectomy—removes all or part of the lower jaw (mandible)
- maxillectomy—removes all or part of the upper jaw (maxilla).
The type of surgery you have will depend on how close the cancer is to any major blood vessels and your brain.
Types of surgery for nose and sinus cancer include:
- craniofacial resection—removes any sinuses and/or bones of the face and head affected by cancer
- maxillectomy—removes part (or all) of the upper jaw (maxilla) and may also remove the top teeth, part of the eye socket, and/or the nasal cavity
- orbital exenteration—removes the eye and surrounding tissue
- rhinectomy—removes all or part of the nose
- endoscopic sinus surgery—removes tissues of the nasal cavity and sinuses using an endoscope that is inserted through a nostril.
The type of surgery you have will depend on which salivary glands are affected by the cancer.
Surgery to remove salivary glands can be difficult because many of the nerves of the face and neck are very close to these glands.
Any surgery used to treat salivary gland cancer will remove either all or part of the affected gland and some of the surrounding tissue. Sometimes the surgeon will also remove any nearby lymph nodes.
The type of surgery will depend on the size of the cancer and where in the throat it is.
Types of pharyngeal surgery include:
- pharyngectomy—removes part (or all) of the pharynx (throat)
- oropharyngectomy—removes some of the oropharynx (the middle part of the throat that starts behind the mouth)
- hypopharyngectomy—removes part of the hypopharynx (the bottom part of the throat that sits behind the voice box (larynx))
- laryngopharyngectomy—removes the voice box (larynx) and most of the pharynx.
Laryngeal cancer affects the larynx. Your larynx is more commonly called your voice box.
Three types of surgery may be used depending on the size and location of laryngeal cancer.
- Endoscopic resection—used in early-stage laryngeal cancer. Surgery is done using an endoscope.
- Partial laryngectomy—removes part of the voice box. You may need a temporary tracheostomy (breathing tube) during your recovery.
- Total laryngectomy—removes the larynx and sometimes nearby lymph nodes. You will have a hole (stoma) left in your neck to help you breathe. See page 60 for information on tracheostomy.
Ways to talk after a laryngectomy
After a partial laryngectomy you will still have part of your voice box, but you may have some problems with your voice and swallowing.
After surgery to remove your voice box, you will no longer have vocal cords to create a voice, and you may need to learn to speak again in a different way.
Mechanical speech
A battery-powered device called an electrolarynx is used to create a mechanical voice. The device is held against your neck or cheek or placed inside your mouth. You press a button on the device to make a vibrating sound.
Tracheoesophageal puncture speech
The surgeon creates a small hole between your trachea (windpipe) and oesophagus (food tube). A small voice prosthesis or valve is inserted to direct air from your trachea to the oesophagus. This creates a low-pitch, throaty voice.
Oesophageal speech
You swallow air and force it up through your oesophagus to produce a low-pitched sound. This technique can be difficult and needs training with a speech-language therapist.
Surgery is the main treatment for cancer that starts in the skin. The type of surgery will depend on the type and stage of cancer.
Surgery is the most common treatment option for thyroid cancer. It can include:
- hemithyroidectomy—removes half of the thyroid
- total thyroidectomy—removes all of the thyroid
- neck dissection—see below.
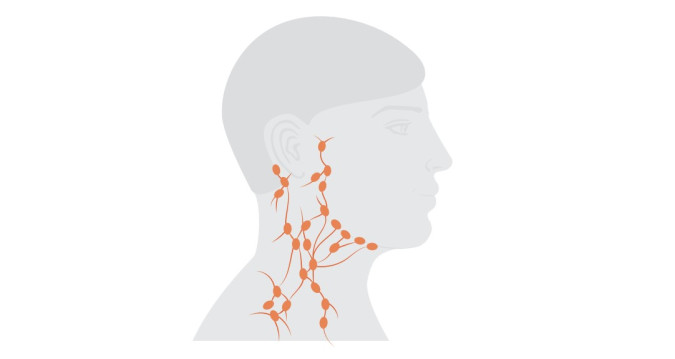
Lymph nodes are small, bean-shaped glands that are found throughout the body. They contain immune cells to help the body fight infection. Lymph nodes also filter lymph fluid. There are more than 300 lymph nodes in the head and neck.
Your cancer treatment team may recommend removing some (or all) of the lymph nodes from one side, or sometimes both sides, of your neck. This surgery is called a neck dissection.
This may be done if:
- tests show that cancer has already spread to the lymph nodes
- there is an increased risk of the cancer spreading to the lymph nodes.
This image was produced by Macmillan Cancer Support and is reused with permission.
If a large area of tissue is removed during surgery, you may need additional surgery to rebuild (reconstruct) the area. This is called reconstructive surgery. It is also done if surgery is likely to affect how you swallow or how you look.
You can have reconstructive surgery using:
- a skin graft—a thin piece of skin is taken from another part of your body to cover the place where the cancer has been removed
- a flap repair—skin, and the tissue that is under it, is taken from another part of your body, e.g. your thigh, arm, back, or tummy (abdomen), and attached to the area where the cancer has been removed
- a bone graft—bone from another part of the body (usually the lower leg) is used to replace the area of bone that has been removed. This may be needed if the cancer is in the jawbone
- an artificial replacement—this is known as a prosthesis and uses material such as titanium or silicone to re-create areas such as bones in the face or palate that have been removed. E.g. a dental plate called an obturator can be used to cover gaps in the roof of the mouth.
Recovery from surgery to treat head and neck cancer may take a long time. Your treatment team will talk to you about the benefits and side effects of surgery.
Depending on the type of head and neck cancer, some people recover fully and can gradually return to their usual activities. For others there may be longer-term changes to their appearance and to how they speak, eat, and drink.
Your treatment team may refer you to a rehabilitation service, where you will receive support such as speech-language therapy or physiotherapy. This can help in your recovery and teach you ways to manage any changes you have. Counselling services can also help you to adjust to these changes.
Radiation treatment
Radiation treatment is the use of X-ray beams to destroy cancer cells or slow their growth. Radiation treatment only affects the part of the body that the beams are aimed at.
Radiation can be used:
- on its own as the main treatment for pharyngeal and laryngeal cancer
- after surgery (adjuvant) to treat any cancer cells not removed with surgery and to reduce the chance of the cancer coming back
- with chemotherapy (chemoradiation) to increase the effects of the radiation
- to improve your quality of life or extend your life (palliative treatment)
- to treat cancer that has spread to other organs such as the brain or bones (palliative treatment).
External beam radiation treatment is given from outside the body by a machine called a linear accelerator (LINAC). This is the most commonly used type of radiation treatment for head and neck cancer.
Treatment is given daily (Monday to Friday) and your treatment team will give you information on how long you will have treatment for. The LINAC is on for only a few minutes and the total time spent in the treatment room is usually 10 to 20 minutes.
Treatment is carefully planned to do as little harm as possible to your normal body tissue.
Sometimes radiation treatment and chemotherapy are used together. This is called chemoradiation. Combining the treatments can make the side effects of radiation treatment worse.
If you are having radiation treatment to your head and neck, you will have a mask made to keep your head completely still and in the right position for treatment. It will be made of plastic mesh, so you will
be able to see and breathe through it.
Some people find that the thought of wearing a mask throughout treatment makes them feel anxious or claustrophobic. If you have any concerns, talk to your treatment team, as they are experienced in helping people to manage this.
Image taken from Cancer Society of New Zealand radiation treatment booklet
Radiation treatment is available at specialist treatment centres in Auckland, Hamilton, Tauranga, Palmerston North, Wellington, Christchurch, and Dunedin (2023).
If you need to be away from home for your treatment, help may be available for transport and accommodation costs through the National Travel Assistance Scheme.
Your treatment centre, hospital social workers, the travel office at your local hospital, or your local Cancer Society can advise you on what help may be available.
You can find more information about the National Travel Assistance Scheme on our website: Find more information about the National Travel Assistance Scheme
Side effects of radiation treatment for head and neck cancer
People react to treatment in different ways. Side effects are usually temporary, but some may last for several weeks to a few months. They may also be permanent.
These are the common side effects.
- Fatigue (tiredness)—can occur during and after treatment
- Mouth sores
- Dry mouth
- Thick saliva
- Painful swallowing
- Difficulty breathing
- Red and dry skin in the area being treated
- Loss of appetite
- Hair loss in the area being treated
Chemotherapy treatment
Chemotherapy is medication used to kill cancer cells or slow their growth. It
affects cells throughout the body.
You may want to read the booklet Chemotherapy/Hahau, available on our website or phone the Cancer Society Information Helpline at 0800 CANCER (226 237) to ask for a copy to be sent to you.
Chemotherapy may be given:
- before surgery or radiation treatment to try to shrink the cancer (neoadjuvant)
- alongside radiation treatment (chemoradiation) to increase the effectiveness of the radiation treatment
- after surgery to reduce the chances of the cancer coming back (adjuvant)
- as palliative treatment to reduce symptoms and improve your quality of life or extend your life.
Chemotherapy is given through a vein (IV) or as tablets. If it is given through a vein, it may be given through a cannula. A cannula is a small tube that is put into a vein in your arm or the back of your hand and is removed after each treatment.
Some people need a central venous access device (CVAD) such as a portacath or a peripherally inserted central catheter, which stays in place for the whole of their treatment. It is a fine tube placed in the arm or chest that ends in the large veins inside the chest.
For more information on CVADs, see the Cancer Society’s Chemotherapy, Immunotherapy and Targeted Treatment booklet, available on our website:
IV treatment is usually given to you as an outpatient at your local treatment centre, at regular intervals over several months. Not all people with head and neck cancer will receive the same treatment.
The chemotherapy side effects depend on the combination of medications you receive. Common side effects that you may experience include:
- increased risk of infection
- increased risk of bleeding or bruising
- reduced immunity
- hair loss
- infertility
- fatigue
- forgetfulness and concentration problems (chemo brain)
- nausea and vomiting
- constipation or diarrhoea
- hearing loss
- numbness and tingling in the hands and feet (peripheral neuropathy)
- sore mouth and ulcers.
Some side effects of chemotherapy can be life threatening. If you develop any of the following symptoms, you must contact your treatment team or go immediately to your nearest hospital emergency department and tell them you are receiving chemotherapy treatment.
- Fever—a temperature over 38˚C
- Chills—shivers or shakes, feeling hot or cold
- Chest pain
- Difficulty breathing
- Vomiting that continues after taking anti-sickness medication
- Diarrhoea
- Gum or nose bleeds, or bleeding that does not stop
- Pain or burning when passing urine, or blood in urine
It is important that you do not wait to seek assistance until the next morning or after the weekend.
The availability of targeted treatment and immunotherapy for head and neck cancer
There have been recent advances in head and neck cancer treatment.
Unfortunately, these treatments are expensive and Pharmac has decided not to provide funding for all the treatments that might be helpful for the management of your cancer. You may like to ask your oncologist if there are any unfunded treatments or clinical trials available that may be beneficial for you. Your medical oncologist can give you an estimate of the cost involved if you choose to fund your own treatment.
Targeted treatment
Targeted treatment targets the damaged genes or proteins of cancer cells to stop the cancer growing and spreading. It is sometimes called biological therapy.
For more information about targeted treatments, see the Cancer Society’s Chemotherapy, Immunotherapy and Targeted Treatment booklet, available on our website:
Read more about targeted treatment
Targeted treatment medication travels through the bloodstream. Each medication blocks a specific target, e.g. a damaged gene or protein, on or within a cancer cell. Blocking these targets can kill cancer cells or slow their growth. The signs and symptoms of cancer reduce or disappear and damage to healthy cells is minimal.
If your cancer contains a change (mutation) in a specific gene or protein that is helping your cancer to grow, you may benefit from targeted treatment. To find out if your cancer contains these changes, your doctor will take a tissue sample from your cancer and send it to a laboratory for molecular testing. It may take anywhere from a few days to a few weeks to receive the results.
In New Zealand, Cetuximab is available and funded to treat locally advanced squamous cell carcinoma (SCC) of the head and neck when people cannot receive the standard chemotherapy medication. It attaches to the surface of the cancer cells to prevent them growing and dividing and is used alongside radiation therapy (2023).
Although targeted treatment reduces harm to healthy cells, it can still have side effects. These depend on the medication used and how your body responds. Some people do not experience any side effects and others have more than one. The more common side effects include:
- skin problems—redness, dryness, flaky skin, rash and swelling
- sore mouth and mouth ulcers
- fatigue
- diarrhoea
- an increase in blood pressure
- problems with bleeding and bruising.
Immunotherapy
Immunotherapy is a type of cancer treatment that helps your own immune system to fight cancer.
For more information about immunotherapy, see the Cancer Society’s Chemotherapy, Immunotherapy and Targeted Treatment booklet, available on our website:
Your immune system protects you from infections by killing bacteria and diseases. It also helps to fight cancer. A T-cell is one type of immune cell that does this.
Sometimes part of your immune system is ‘turned off’ so it no longer recognises the abnormal cell growth that causes cancer. Immunotherapy helps to ‘turn on’ this part of your immune system so that it can identify and attack cancer cells.
Currently in head and neck cancer treatment, immunotherapy is mostly used for people who have advanced cancer. Sometimes it is used following chemotherapy and radiation treatment where the aim of the treatment is to cure the cancer. It is not yet as widely used as chemotherapy and radiation treatment.
In New Zealand, checkpoint inhibitor immunotherapies pembrolizumab (Keytruda) and Nivolumab (OPDIVO), have been approved for use for some people with squamous cell carcinoma (SCC) of the head and neck. These treatments are not currently funded in New Zealand (2023).
Immunotherapy is not suitable for everyone, so talk to your treatment team about whether you might benefit from it.
The side effects of immunotherapy depend on the type of treatment you receive and how your body responds. They will be different from those of other cancer treatments. Immunotherapy can cause flu-like symptoms and your immune system to be over-active, resulting in a range of side effects. This is your body’s expected response to the treatment. The more common side effects include:
- Fatigue
- Dry eyes
- Skin rash
- Diarrhoea
- Joint pain.
Supportive care and palliative treatment
Anyone with head and neck cancer may need supportive care. That includes the management of physical symptoms, emotional and spiritual support, and guidance to help them plan ahead.
Supportive care is mostly provided by primary health care teams, Cancer Society support workers, and palliative care services.
An important part of planning ahead is preparing an advance care plan. Advance care planning helps you, and the people important to you, to talk about the treatment and care you may want towards the end of your life. It will guide your whānau and doctors when you can no longer tell them yourself.
Advance care planning is voluntary—no one can force you to do it.
You may need extra support if the symptoms you are experiencing are complex or difficult to manage. Your primary care team may refer you to a specialist palliative care service.
Palliative care is often provided by primary health care teams as part of supportive care. It is a good idea to ask for palliative care early rather than wait until things become difficult to manage. This can help to reduce stress for you and your whānau.
Specialist palliative care can be offered at home or in a hospital, rest home, or hospice. Coordinated care is provided by specialist doctors, nurses, social workers, spiritual care workers, and cultural health services. Their services include, for example, helping you with physical and emotional symptoms and helping you to get practical support.
You may also be faced with decisions that are hard to make during your illness. The specialist palliative care team may be able to explain things to you and help you to find answers. In general, specialist palliative care services are free. There may be a charge for hiring some equipment if you are being cared for at home.
Traditional treatments
Traditional healing has been a central part of Māori culture for generations. Values, belief systems, and teachings from kaumātua and tohunga have seen Māori focus on total wellbeing, which includes taha tinana, taha hinengaro, taha wairua and taha whānau (the physical domain, the domain of the mind and behaviour, the spiritual domain, and the whānau or social domain).
Traditional healing methods can include rongoā Māori, romiromi and mirimiri—therapies that are based on the use of native plants, massage therapy, and spiritual healing.
Traditional healing is also important to Pacific peoples, to help in their recovery. It takes a holistic approach to treating the person, where mental, emotional, physical, and spiritual needs are looked after together, rather than as separate parts. The treatment offered to each person depends on their specific needs. Medicinal plants and herbs may be used during the treatment process, as well as stones and massage.
If you are thinking about using either Māori or Pacific traditional healing, please discuss it with your cancer treatment team. Both traditional healers and your treatment team aim to provide you with the best possible care that has minimal side effects. If you have difficulty expressing your needs to your treatment providers, find someone to advocate on your behalf. Then the traditional healers and hospital treatment specialists can work together to support you on your cancer journey.
Other treatments
It is important to discuss any additional treatments you are using or thinking of using with your treatment team. Some treatments may be harmful if they are taken at the same time as medical treatments, so it is advisable to discuss the benefits, medicine interactions, and any safety concerns.
Other treatments
Complementary treatments (sometimes called integrative therapy) are healing practices and products that are not usually part of standard medical care. A few practices are now being used to complement medical treatments. Examples include massage, meditation, and acupuncture, which are sometimes used to lessen the side effects of treatment.
When these treatments are used instead of medical treatment, they are considered alternative treatments. Some alternative therapists may claim their treatments are cancer cures—this is very unlikely to be true.
You can check for warnings on natural and herbal products on the Medsafe website:
For more information on complementary and alternative medicine, see the Cancer Society’s Complementary and Alternative Medicine booklet, available on our website:
