An A-to-Z guide to managing symptoms and side effects of head and neck cancer.
Download the complete head and neck cancer booklet
Our new booklet 'Understanding head and neck cancer' is available now.
Download section seven of our head and neck cancer booklet: An A-to-Z guide to managing symptoms of head and neck cancer

A
Changes to your appearance may leave you feeling less confident, especially if you have had surgery to remove part of your face or jaw.
Sometimes reconstructive surgery can be done. This aims to give you the best possible function and appearance after treatment. Surgical scars will fade in time and are often planned to fit into the natural lines of your face and neck.
Your treatment team will talk to you about the changes you may experience after treatment. They can also suggest ways to help you cope with any changes and refer you to support services as needed.
You may like to get in touch with the Look Good Feel Better programme. This free programme for men and women explains how to use skin care, hats, and wigs to help restore appearance and self-esteem during and after treatment.
Some treatments to the head, neck, nose, and mouth may affect your appetite.
After some treatments you may lose your sense of taste. Other people find that food can taste salty or metallic. This can affect your appetite, and you may lose weight.
Your sense of appetite may improve slowly over several months. Sometimes it is a permanent change.
Making food look appealing, or using different textures, may help to improve your enjoyment of food. A dietician or speech-language therapist may be able to help.
Tip: Try a nutritional supplement drink if you have lost your appetite for food or you are finding it difficult to eat.
Sometimes surgery that removes the lymph nodes in your neck can affect the nerves in your shoulder. This can make your arm feel weak and your shoulder stiff. It usually resolves over time. A physiotherapist will be able to give you exercises to help improve your strength.
B
Depending on the location of the cancer, you may have difficulty breathing. People with nasal cancer may find it hard to breathe through the nose. People with cancers of the throat and larynx may feel it is hard to get enough air in.
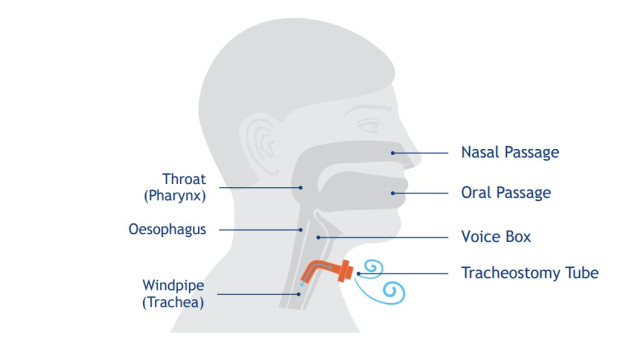
To help you breathe you may need a tracheostomy (breathing tube) at the front of
your neck. This may be:
- temporary—to help bypass the cancer or after radiation treatment if your throat swells
- permanent—if your voice box (larynx) has been removed (laryngectomy).
What is a tracheostomy?
A tracheostomy is a small hole in the lower part of your neck that goes directly into your trachea (windpipe). It is held open by a small plastic tube.
While you have a tracheostomy, you cannot usually talk with the tube in place. You will need a pen and paper, a mobile phone, or a laptop to communicate.
If you need a permanent tracheostomy, a speech-language therapist will teach you how to talk and swallow.
A physiotherapist will show you exercises and ways to clear your airway to help when you have a cold or cough.
D
If you need any teeth removed, this will need to be done before starting radiation treatment to allow time for the gums to heal. It is not unusual to have ongoing problems with your teeth after head and neck treatments due to a lack of saliva. Saliva cleans and protects teeth from decay. Using a daily fluoride toothpaste or mouthwash will help. You should see your dentist for a checkup every 4-6 months.
Drinking water, chewing sugar-free gum, and avoiding sucking sugary sweets or drinks will help prevent decay. It is also important to brush your teeth several times a day with a soft toothbrush.
Low mood or depression can be common when you have head and neck cancer, especially if you have experienced physical changes such as a change in your facial appearance or the permanent loss of sight, taste, or smell, or you are unable to communicate like you did before.
If you or the people around you are concerned about how you may be feeling, talk to your treatment team or GP or whānau doctor for support. Counselling may be useful to help you adjust to some of the changes or feelings that you are experiencing.
A dry mouth can be caused by radiation treatment to the head and neck and may be permanent. A dry mouth makes it harder to keep your mouth and teeth clean.
Saliva protects teeth and gums, so a lack of saliva may increase tooth decay. Using
a fluoride toothpaste and simple salt and bicarbonate of soda mouth wash
regularly may help.
Tips:
- Ask your treatment team about products such as artificial saliva, enzyme gels, mouthwashes, lozenges, and lubricants to help keep your mouth and lips moist.
- Try sipping cool drinks during the day. Carry a bottle of water with you. Avoid sugary, alcoholic, or acidic drinks.
- Avoid very dry food like crackers.
- Use sauces or gravy to make food moist and easier to swallow.
- Avoid sucking sugary lollies; instead, try sugar-free gum to reduce tooth decay.
- Smoking can make a dry mouth worse, so try to give up or cut down.
F
If the nerves in the face are damaged during treatment, it can affect how the muscles in your face move. You may be unable to smile, frown, or close an eye, or your face may droop.
Depending on the area that is affected, the way your face moves and how it looks might be able to be improved with procedures such as nerve transfers and Botox injections. This will only be considered once you have recovered from treatment.
Fatigue can be described in many ways, including feeling exhausted, extremely tired, sleepy, or drowsy, or finding it difficult to concentrate. Fatigue can appear suddenly, and rest may not help. Here are some ideas to help you cope with fatigue.
- Let people help you. Family, friends, and neighbours may offer to help with tasks such as shopping, childcare, housework, and driving.
- Take a few weeks off work during or after treatment, or work fewer hours. You may be able to work from home.
- Do light exercise, such as walking, and keep up your normal exercise routine if approved by your doctor. Do not start any new exercise routine until you feel better after treatment.
- Try to eat a healthy, well-balanced diet. Some people find small, frequent snacks more appealing than trying to eat a meal. If you have nausea, have your meals when you feel like eating.
- Fatigue may be caused by some specific things that can be found in blood tests and may be improved by treatment.
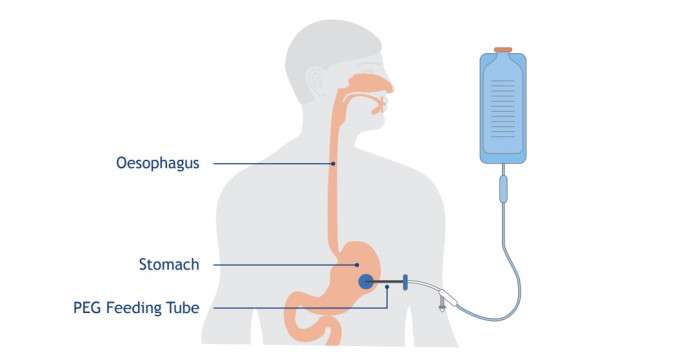
If you are unable to eat and drink, your treatment team may suggest you have a feeding tube put into your stomach to make sure you get enough nutrition. This is usually temporary but, in some cases, it may be permanent.
Feeding tubes can be managed at home with support and guidance from your treatment team.
The most common type of feeding tube used in head and neck cancer is called a PEG (Percutaneous Endoscopic Gastrostomy) tube. The PEG tube goes into your stomach through an opening made on the outside of your tummy (abdomen).
Your dietician will prescribe special liquid nutrition that will go straight into your stomach through the PEG tube. You will be told what other fluids and medications can be put through the PEG tube.
© Cancer Research UK [2002] All rights reserved. Information taken 2023
Some cancer treatments can affect your fertility, so you may not be able to have children in the future. Depending on your age and wishes before treatment, there may be some fertility-preservation options available. Ask your treatment team about fertility as early as possible, as it may mean you have more options for protecting or preserving yours.
H
Your hearing may be affected by surgery or chemotherapy. You may experience hearing loss or difficulty hearing high-pitched sounds, or hear a ringing or buzzing sound (tinnitus). If you notice any changes in your hearing, let your treatment team know straight away.
If your hearing loss is likely to be permanent, your treatment team can refer you to an audiologist (a person trained in hearing loss). They will test how much hearing loss you have and recommend ways to help.
Getting used to changes in your hearing can take time, but there are some things you can try that may make it a little easier.
Tips:
- Let people know that your hearing is not as good as it used to be and ask them to look at you when you are talking with them.
- Try to reduce background noise (TV, radio) when you are talking with people.
- If you are in a group situation, sometimes asking one person to relay the conversation to you may be helpful.
If you are experiencing tinnitus, Tinnitus Australia has a lot of useful self-help tools and information available on its website.
I
Head and neck cancer can affect your sexuality in emotional and physical ways.
Treatment for head and neck cancer can affect your self-esteem and ability to express your desires, and make kissing or oral sex difficult or less enjoyable.
See our booklet on sex and cancer
If the cancer was HPV related (see page 18) you and your partner may be worried about them getting HPV from sex. Research shows it is not usual for long-term partners of people with oral HPV to get HPV related cancer themselves. New partners may be at risk and may want to use condoms, but for most people the virus is cleared by the immune system. Read more about HPV here
J
Jaw stiffness (trismus)
Sometimes radiation treatment and/or surgery cause some face muscles to become stiff. This is called trismus.
The stiffness can mean that you are not able to open your mouth wide. This can affect eating, speech, and oral hygiene.
A speech-language therapist can show you some simple mouth-opening exercises to help keep your mouth and jaw as flexible as possible.
Changes to the jawbone (osteoradionecrosis)
Radiation treatment to the head and neck can sometimes affect the blood supply to the jawbone. If the bone is further damaged by surgery or the removal of teeth, or if dentures are irritating the jawbone, a very rare condition called osteoradionecrosis can develop.
If you notice any problems with your teeth or gums, or swelling, pain, heaviness, or numbness in your jaw after radiation treatment, it is important to get it checked immediately by your GP or whānau doctor or your dentist.
L
Lymphoedema is swelling in an area of the body caused by the lymph vessels being removed or blocked. It is a long-term side effect of some treatments for head and neck cancer.
If you have had radiation treatment or surgery to remove lymph nodes, there is a risk of developing lymphoedema in your face and/or neck. The risk increases if both sides of your neck have been treated. Sometimes the symptoms of lymphoedema can take months or years to develop, although some people who are at risk never develop it.
The main symptoms of lymphoedema may come and go. They include swelling and redness, and your skin may feel warmer to touch.
Sometimes the swelling develops internally and is hard to see. If this happens, the area may feel different—some people describe it as a mild tingling sensation.
Lymphoedema is easier to manage if it is treated early, so it is important to see your GP or whānau doctor if you notice any of these symptoms.
The best treatment for lymphoedema is a programme of exercise, massage, skin care and medical taping, and sometimes a properly fitted compression garment. Damage to the lymph nodes means it is not usually possible to reverse the swelling, so the aim of treatment is to manage the swelling on a long-term basis.
To find a lymphoedema therapist near you, follow the link to the Lymphoedema New Zealand website:
Lymphoedema New Zealand websiteLiving with lymphoedema information sheet
M
Soreness in the mouth is commonly called oral mucositis. It is often caused by chemotherapy and radiation treatment.
Mucositis can make any part of your mouth red, sore, and ulcerated. It is painful and can make eating, swallowing, and talking difficult.
Your treatment team can prescribe medications to help reduce the pain. If the pain is not well managed and you are having difficulty eating or drinking, let your treatment team know. They may recommend a feeding tube for a short period of time until treatment ends.
If you have a sore mouth, the following suggestions may be useful:
- Try eating soft or pureed foods, such as soup, smoothies, and yoghurt.
- Avoid eating hot, spicy, or very cold food and drink.
- If eating and drinking is painful, you may benefit from a nutritional supplement drink. Talk with your dietician to get the right supplement for your needs.
- Use a salt and bicarbonate mouthwash regularly throughout the day.
- Keep your teeth, gums, and mouth clean using a soft toothbrush and fluoride toothpaste to reduce the risk of a mouth or throat infection.
- Take pain relief before meals as prescribed.
- Avoid alcohol and tobacco as they can irritate the lining of your mouth and throat.
Mouthwash recipe:
- Add 1 tsp of salt and 1 tsp of baking soda to 1 litre of water
- Mix well until dissolved.
- Store in the fridge and discard after 24 hours.
- Use as a mouthwash and rinse mouth as required. Spit it out—do not swallow.
The mix is a good cleanser. It helps healing, helps to break down thick saliva, and reduces tooth decay.
Use often during the day, after food, and before going to sleep at night.
N
People with head and neck cancer may find eating difficult and experience weight loss. Eating well can increase your energy and helps you to cope with the side effects of treatment.
If you are unable to eat and/or drink enough to meet your nutritional needs, you will be referred to a dietician for individual support. If you have tried increasing your food and fluid intake but are still finding it difficult, your dietitian may suggest you try using nutritional supplement drinks. Some supplement drinks are available from supermarkets, and others from pharmacies. You may be able to get prescriptions for some of these after an assessment by your dietician.
If your nutritional needs are still unable to be met, your treatment team may suggest a feeding tube.
P
Not everyone will have pain or discomfort that continues after treatment. If you do, it can usually be well managed by taking pain-relieving medications regularly. Tell your treatment team if the pain continues so they can help.
If lymph nodes are removed or treated with radiation therapy, you may have pain, stiffness, and numbness in your neck and shoulder. This may make neck movements like lifting an arm difficult.
Ask your treatment team or physiotherapist for exercises to help manage and reduce the pain. They may suggest ways of positioning your body to reduce pain and stiffness. Sometimes the numbness will be permanent.
S
Some treatments to the head, neck, nose, and mouth may affect your sense of smell.
If you have had surgery to remove cancer from the bones of your face, or your sinuses, you may lose your sense of smell.
Your sense of smell may improve slowly over several months. Sometimes it is a permanent change.
Making food look appealing, or using different textures, may help to improve your enjoyment of food. A dietician or speech-language therapist may be able to help.
Tips:
- Use ready-made meals or ask someone else to cook for you if cooking smells bother you.
- If losing your sense of smell has decreased your appetite, you may want to try a nutritional supplement drink
- If your sense of smell has changed:
- check food expiry dates
- check regularly that the smoke detectors in your home are working.
Your ability to talk may be affected by the cancer and/or cancer treatment. After treatment, you may lose the ability to speak clearly or experience changes in your voice. These changes will depend on where the cancer is located and the type of treatment you have.
Tips:
- Work with a speech-language therapist to improve your speech and learn strategies for communicating with your family and friends.
- Do speech therapy exercises to improve the strength and range of motion of your lips, tongue, jaw, and larynx.
- Use technology (e.g. a computer, tablet, or mobile phone) to write and send notes. NZ Relay helps people who have difficulty speaking to connect with friends and whānau over the phone.
Your mouth may now have mucus that is thick and sticky. Keeping your mouth clean and moist and using a salt and baking soda mouthwash regularly may help. Have tissues ready in case you wish to spit out the mucus. Should the mucus change colour to green/yellow/brown tell your GP/whānau doctor or treatment team.
After a neck dissection you may have stiffness or weakness in your shoulders. This is because the nerve that helps shoulder movement may have been affected by surgery. A physiotherapist will give you exercises you can do to help improve this.
Many people with head and neck cancer have problems swallowing (dysphagia). Signs of difficulty in swallowing may be:
- you are taking longer to chew and swallow food
- you are coughing or choking while drinking or eating
- food is sticking in your mouth.
You may have trouble swallowing before, during, and after treatment and it may be caused by the cancer itself or the treatment. Ask to see your speech-language therapist early in your treatment so they can support you with exercises and techniques to help keep your swallowing safe.
Swallowing and chewing involves the lips, teeth, tongue, and muscles of the mouth, face, jaw, and throat. Swallowing is an important function to help maintain weight.
If you are finding it difficult to swallow, you may like to:
- speak to a speech-language therapist
- talk with a dietitian or a speech-language therapist about the best foods to eat and different textures to try
- ask if there are any medications you could try to help reduce any pain you have when swallowing
- do face and mouth exercises regularly to improve the muscles in your head and neck
- if it is safe, continue to eat and/or drink during treatment to keep the muscles that help you to swallow working.
T
Some treatments to the head, neck, nose, and mouth may affect your sense of taste. Your sense of taste may improve slowly over several months, but sometimes it will change permanently.
Making food look appealing, or using different textures, may help to improve your enjoyment of food. A dietician or speech-language therapist may be able to help.
Tips:
- Try adding fresh herbs or flavourings to food.
- Clean your mouth and teeth before and after eating.
- If you are a smoker, stopping smoking will help to improve your sense of taste.
See "Jaw stiffness"
V
If an eye has been removed, the empty eye socket will be replaced with a sphere of tissue from another part of your body. This is temporary and is used to keep the shape of the eye socket so you can be fitted with an artificial eye when you have recovered from surgery.
You will still be able to see with your remaining eye, but your peripheral (side) vision and depth perception will change, and your balance may be affected. These changes should not prevent you from continuing activities such as driving and playing sports, but they may take time to get used to.
Before you start driving again you may need a medical certificate from your doctor or optician for Waka Kotahi NZ Transport Agency.
W
The side effects of cancer and its treatments can make it hard to maintain your weight.
Even a small amount of weight loss over a short period of time can cause malnutrition.
Malnutrition is when you are not able to get enough vitamins and nutrients from the food you eat to keep your body healthy and to maintain your weight. Making changes to your diet and adding a supplement drink may be all you need. Some people need additional support to help maintain their nutrition, such as feeding tubes.
Tips:
- Let the treatment team know if you are losing weight or in pain or have problems swallowing.
- Try eating several small meals throughout the day rather than three large ones.
- Try to eat high-energy, high-protein foods at each meal or snack, e.g. drink milk or add cheese to meals.
- Talk to your treatment team or a dietician if you are having difficulty maintaining your weight. They will be able to talk to you about the different nutritional supplements that are available.
Questions you may wish to ask
When you find out that you have head and neck cancer, you and your whānau may have many questions.
Here is a list of questions you may want to ask to help you make the most of your time with your doctor. Let them know if there are things you do not want to be told.
• What type of head and neck cancer do I have?
• What grade is it?
• What scans do I need?
• What treatment do you advise for my head and neck cancer, and why?
• Are there any private treatments available that you would advise for my
cancer, and why?
• Are there other treatment choices for me?
• Are there any clinical trials that I could be eligible for?
• What are the risks and possible side effects of each treatment?
• Will I have to stay in the hospital, or will I be treated as an outpatient?
• How long will the treatment take?
• How much will it affect what I can do?
• How much will the treatment cost?
• If I need further treatment, what will it be like and when will it begin?
• How often will my check-ups be and what will they involve?
• Are there any problems I should watch out for?
• If I choose not to have treatment either now or in the future, what services are
available to help me?
• When can I return to work?
• When can I drive again?
• Will the treatment affect my sexual relationships?
• Is my cancer hereditary (passed on by my parents)?
• Is the treatment attempting to cure the cancer or not?
• What is my prognosis (future outlook)?
• I would like to have a second opinion. Can you refer me to someone else?
If there are answers you do not understand, feel comfortable saying:
• “Can you explain that again?”
• “I am not sure what you mean” or
• “Could you draw a diagram or write it down?”
You can find more information in our Questions You May Wish to Ask booklet, which has general questions and spaces in which you or your doctor can write answers. You can also phone the Cancer Information Helpline (0800 CANCER 226 237) for further information or visit our website:
